Anaemia in the Perioperative Pathway
Anaemia is associated with adverse perioperative outcomes and is present in a third of patients having major surgery
Anaemia is associated with adverse outcomes of surgery. The blood loss of surgery or trauma can cause or worsen anaemia. People who have anaemia have a worse result from their operation including poorer wound healing, slower mobilisation and an increased risk of death. Risk ratios in the published literature suggest people with anaemia have two or three times the rate of complications. Anaemia is often associated with other conditions, but as an independent risk factor, anaemia is responsible for around 20% more complications Interventional studies adopting a Patient Blood Management (PBM) approach, including addressing anaemia, lead to reduced blood transfusion, length of stay, complications and hospital costs.
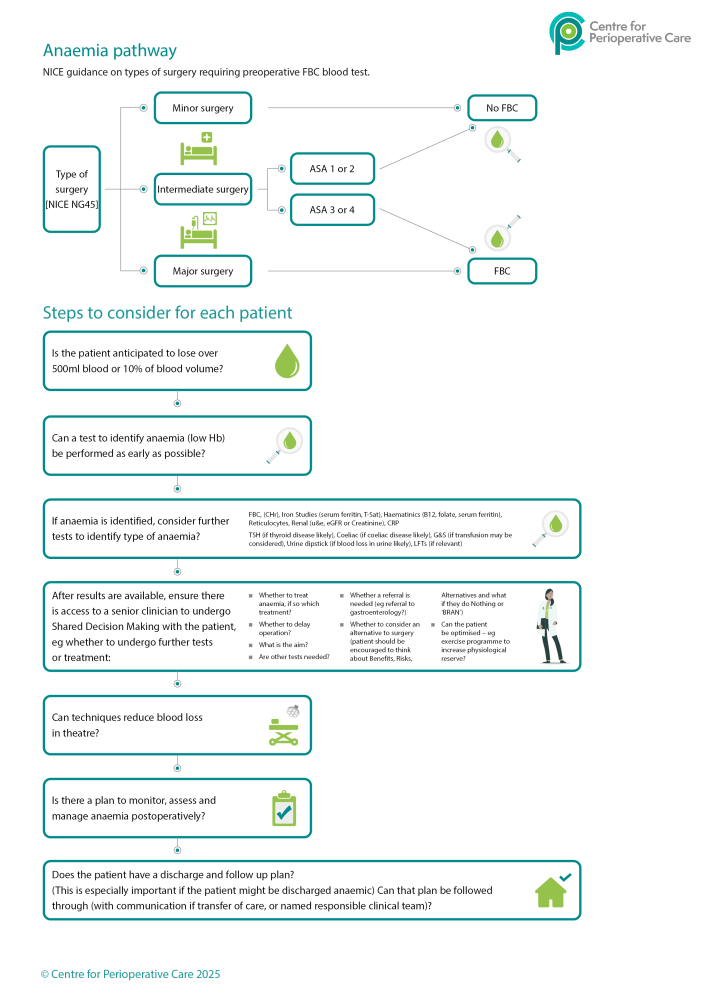
Anaemia is frequently diagnosed late in the work up of patients for surgery. It is increasingly apparent that a pathway approach to care works best. Pathways should be set up that allow a Patient Blood management (PBM) approach: anaemia should be diagnosed early and its cause investigated. Treatment should be given, intraoperative blood loss minimised and the patient’s physiological response optimised. The pathway should anticipate potential problems. .
“Anaemia should be viewed as a serious and treatable medical condition, rather than simply an abnormal laboratory value.”
This CPOC perioperative anaemia guideline (updated 2025) has been developed using a whole pathway approach. It contains recommendations for patients of all ages undergoing surgery and for health care professionals in both emergency and elective surgical settings and across specialities.
Why is this guideline important?
The aim of this guideline is to ensure that the patient is at the centre of the whole process, and that everyone involved in their care carries out their individual responsibilities to minimise the risk from anaemia.
Updated Guideline 2025
The guideline underwent a full review and was republished in March 2025. It has since been updated with minor amendments in May and November 2025. A summary of the changes following the full review can be downloaded for information.
To make the best of this approach we need to make sure patients and all health care professionals including GPs and multidisciplinary hospital teams work together to:
- identify anaemia early in the pathway
- make the patient aware of this and all actions going forward
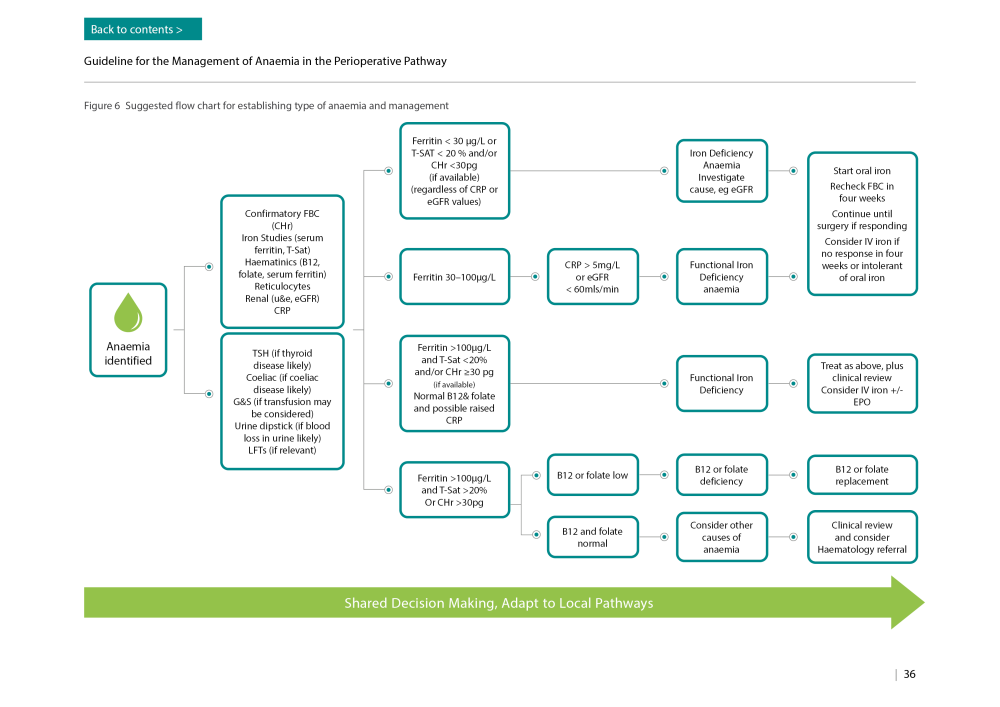
- find the cause of the anaemia
- use tried and tested treatments for anaemia before surgery. This could include advice on changes in diet, oral treatments such as iron supplements and the use intravenous iron when necessary
- make sure the patient has a personalised treatment programme including providing appropriate information about the pros and cons of the different approaches suggested to the patient and how long these should be continued
- communicate clearly between different members of the team so that operations are not cancelled unnecessarily and improve the interface between primary care and hospitals
- talk openly to the patient about the benefits and risks of managing anaemia and the surgery
Recommendations from the Guideline
Resources
- Preoperative intravenous iron therapy: patient information (Cardiff and Vale University Health Board)
- Anaemia patient information (NHS Blood and Transplant)
- Assessment of anaemia (BMJ Best Practice)
- Anaemia, iron deficiency (BMJ Best Practice)
- Patient Information Leaflet – Intravenous Iron (NHS County Durham and Darlington NHS Foundation Trust)
- Iron therapy into a vein (Intravenous) patient information leaflet (Betsi Cadwaladr University Health Board)
- Intravenous iron (University Hospitals Bristol and Weston NHS Foundation Trust)
- Iron in your diet patient information (NHS Blood and Transplant)
- Iron: Food Factsheet (The Association of UK Dietitians) 10 Folic acid: Food Factsheet (The Association of UK Dietitians)
- Iron Supplements: Patient information Factsheet (University Hospital Southampton NHS Foundation Trust)
- Taking Iron Supplements: Information for patients (Oxford University Hospitals NHS Trust)
- Preoperative anaemia management letter: iron supplements (Betsi Cadwaladr University Health Board)
- Preoperative anaemia management letter: intravenous iron therapy (Betsi Cadwaladr University Health Board)
- Preoperative anaemia management letter: oral iron (The Leeds Teaching Hospitals NHS Trust)
- Preoperative anaemia management letter: intravenous iron therapy (The Leeds Teaching Hospitals NHS Trust)
- Patient letter: oral iron tablets (Betsi Cadwaladr University Health Board)
- Patient letter: oral iron tablets (The Leeds Teaching Hospitals NHS Trust)
- Patient letter: intravenous iron therapy (The Leeds Teaching Hospitals NHS Trust)
Supply of ferrous sulphate tablets for the treatment of anaemia (University Hospitals Bristol and Weston NHS Foundation Trust)
My Transfusion is a new app from NHS Blood and Transplant, designed by patients, for patients, to support anyone receiving a blood transfusion.
The app can be downloaded from Google Play store or visit the website here.
Anaemia Guideline Working Group
| Organisation | Name |
| Centre for Perioperative Care | Scarlett McNally |
| Centre for Perioperative Care | Jugdeep Dhesi |
| Centre for Perioperative Care | Steve Evans |
| Association of Anaesthetists | Andrew Klein |
| Association of Surgeons of Great Britain |
Lyndsay Pearce / Hannah Boyd-Carson |
| Association of Paediatric Anaesthetists | Nadia Ladak |
| British Dietetic Association | Rachael Barlow |
| British Society for Haematology | Hafiz Qureshi / Noémi Roy |
| British Orthopaedic Association | Michael Kelly / Mike Reed |
| College of Operating Department Practitioners | Mike Donnellon |
| Federation of Surgical Specialty Associations/ British Association of Urological Surgeons | Duncan Summerton |
| NHS blood and transplant | Frances Sear |
| Patient Representative | Rosalyn Watson |
| Patient Representative | Donna Saunders |
| Patient Representative | Louise Trewern |
| Preoperative Association |
Cathryn Eitel / Anjna Patel |
| Royal College of Anaesthetists | Caroline Evans |
| Royal College of Emergency Medicine | Eleanor Syddall |
| Royal College of Nursing Perioperative Forum | Joanna Holland |
| Royal College of Obstetrics and Gynaecology | Simon Cunningham |
| Royal College of Pathologists | Jennifer Tam |
| Royal College of Physicians Edinburgh | Jennifer Tam |
| Royal College of Physicians | Andrew Goddard |
| Royal College of Surgeons of England | Simon Kendall |
| The British Society of Gastroenterology | Neeraj Bhala |
| Trainee representative | Vatsala Padmanabhan |
| Trainee representative | Laura Blood |
| United Kingdom Clinical Pharmacy Association | Claire Frank |
Download the perioperative anaemia infographic
For summarised steps on how to set up a perioperative anaemia pathway in your hospital.





