Perioperative Care of People with Diabetes Undergoing Surgery
Collaborating to improve care for patients with diabetes
The Centre for Perioperative Care, working in partnership with Diabetes UK, has now published guidance for the care of people with diabetes undergoing elective and emergency surgery that encompasses the whole perioperative pathway
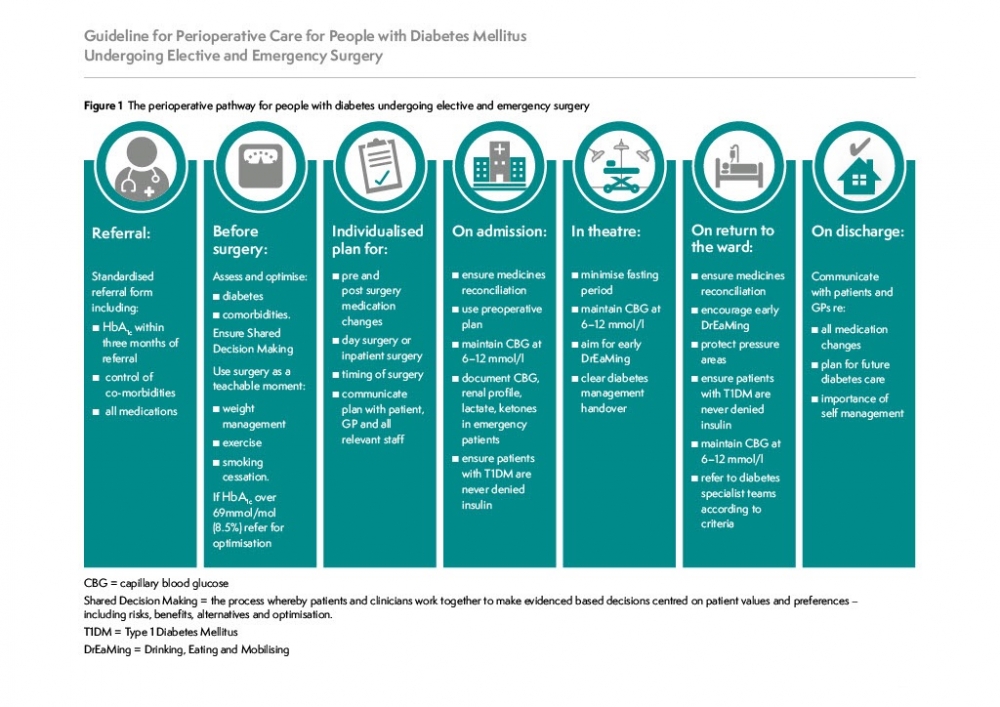
The Centre for Perioperative Care, working in partnership with Diabetes UK, has updated guidance for the care of people with diabetes undergoing elective and emergency surgery that encompasses the whole perioperative pathway. The guidance has been updated and republished in October 2023.
The impetus for the collaboration has arisen from the recommendations of the National Confidential Enquiry into Patient Outcome and Death (NCEPOD) report into the management of patients with diabetes undergoing surgery, Perioperative Diabetes: Highs and Lows. CPOC was commissioned by the Academy of Medical Royal Colleges to develop this guidance
The scope of this guideline covers all aspects of perioperative care relevant to people with diabetes undergoing elective and emergency surgery in adult areas. It is written for clinicians and healthcare professionals involved in delivering care throughout the surgical pathway, as well as for managers and commissioners, people with diabetes and their carers. Implementation of the guideline will require collaboration between all stakeholders, an implementation strategy, workforce development with supporting education and training resource and evaluation through refinement of current national audit tools.
We look forward to working with all of our collaborators to translate these recommendations into routine clinical care.
Structure of the Guidance
Delivering whole pathway, quality perioperative care requires multicomponent intervention, with integration across primary, secondary and social care from the moment surgery is contemplated through to full recovery. A multidisciplinary ‘one team’ approach is necessary to deliver each component of the pathway; shared decision making (SDM); preoperative risk assessment and optimisation of physiological status, co-morbidities and syndromes; lifestyle modification to improve both surgical and long-term health outcomes; quality, targeted postoperative care including rehabilitation; proactive discharge planning; patient and carer involvement, education and empowerment. Delivering such an approach requires accessibility to and effective use of technology, underpinned by research and implementation science.
- Recommendations for organisations
- Recommendations for primary care teams
- Recommendations for staff working in surgical outpatients
- Recommendations for staff working in preoperative assessment services
- Recommendations for staff delivering care during hospital admission for elective surgery
- Recommendations for staff admitting people with diabetes as emergency surgical admissions
- Recommendations for staff in theatre and recovery
- Recommendations for teams delivering postoperative ward care
- Recommendations for safe and effective discharge and follow up
- Recommendations for research
- Recommendations for people with diabetes and their carers and the staff engaging with them
The guideline contains a number of practical resources and appendices to support the multidisciplinary team in the delivery of these recommendations..
Practical resources
| 1.1 | Perioperative management of medications for diabetes: Guideline for perioperative adjustment of insulin |
| 1.2 | Perioperative management of medications for diabetes: Guideline for perioperative adjustment of non-insulin diabetes medication before surgery |
| 2 | Suggested Scales for Variable rate Intravenous Insulin Infusion |
| 3 | Prevention of hypoglycaemia and treatment for ‘looming’ hypoglycaemia and hypoglycaemia |
| 4 | Rescue treatment for perioperative hyperglycaemia |
| 5 | A clinical guideline that facilitates the perioperative use of continuous subcutaneous insulin infusion |
Appendices
| 1 | Roles and responsibilities of clinical lead for perioperative diabetes care in hospitals |
| 2 | Factors to consider in the perioperative management of people with diabetes |
| 3 | Perioperative blood glucose target zones |
| 4 | Indications and use of VRIII |
| 5 | Initial diabetes management of the patient admitted as a surgical emergency |
Most comprehensive, multidisciplinary guidance that has been published on perioperative diabetes care.
Who was involved?
The guidance was developed by the CPOC Diabetes Guideline Working with the following members;
| Ms Goher Ayman | Patient representative |
| Professor Ketan Dhatariya | Joint British Diabetes Societies (JBDS) for Inpatient Care Group |
| Dr Jugdeep Dhesi | Centre for Perioperative Care Deputy Director |
| Professor Dileep Lobo | Royal College of Surgeons of England |
| Ms Agnes Graja | Royal College of Nursing Diabetes Forum Steering Group Committee |
| Professor Mike Grocott | Centre for Perioperative Care |
| Dr Clare Hambling | Primary Care Diabetes Society |
| Ms Andrea Lake | Royal College of Nursing |
| Dr Nicholas Levy | Royal College of Anaesthetists |
| Dr Philip Newland-Jones | United Kingdom Clinical Pharmacy Association (UKCPA) |
| Mr Simon O’Neil | Diabetes UK |
| Dr Helen Parretti | Royal College of General Practitioners |
| Professor Gerry Rayman | Diabetes UK, Get it Right First Time (GIRFT) |
| Dr David Selwyn | Centre for Perioperative Care Director |
| Ms Sarah Tinsley | United Kingdom Clinical Pharmacy Association (UKCPA) |
Resources to Help With the Diabetes Perioperative Pathway
E.Page, R.Allen, F. Wensley, G.Rayman (2020) Improving the peri-operative pathway of people with diabetes undergoing elective surgery. DiabeticMedicine. DOI: 10.1111/dme.14307
Please read the full article here.
Aim
To determine whether outcomes for people with diabetes undergoing elective surgery improve following the introduction of innovations in the peri‐operative care pathway.
Methods
Following a baseline audit of 185 people with diabetes listed for elective surgery (July to December 2017) with a length of stay > 24 hours, a number of changes in practice were implemented. These included dissemination of a ‘diabetes peri‐operative passport’ to participants preoperatively, formation of a diabetes surgery working group, recruitment of surgical diabetes champions and the roll‐out of surgical diabetes study days. Crucial was recruitment of a diabetes peri‐operative nurse, whose role included engaging and educating others and supporting individuals throughout their peri‐operative diabetes care. Records of 166 individuals listed for surgery during the implementation period (July to December 2018) were then audited using the same methodology.
Results
The availability of a recent HbA1c measurement significantly increased (63% vs 92%; P ≤ 0.001). The mean HbA1c of those seen for optimizations by the diabetes peri‐operative nurse significantly decreased [84 mmol/mol (9.8%) vs 62 mmol/mol (7.8%); P ≤ 0.001]. Recurrent hypoglycaemia significantly decreased (7.0% vs 0.6%; P = 0.002) and the mean number of hyperglycaemic events in people experiencing hyperglycaemia almost halved (3.0 vs 1.7; P =0.007). The mean length of hospital stay significantly decreased (4.8 vs 3.3 days; P =0.001) and, crucially, 30‐day readmissions did not increase (12% vs 9%; P =0.307). Postoperative complications significantly decreased (28% vs 16%; P =0.008), including a composite of dysglycaemic complications, poor wound healing, wound infection and other infections (12% vs 5.4%; P =0.023).
Conclusion
The new pathway improved important peri‐operative outcomes for people with diabetes undergoing elective surgery with the potential for cost savings. These findings could have important implications for peri‐operative care on a wider scale.
The 'My Diabetes Passport: Planning For Surgery' allows patients and perioperative teams to document all a patients information during their journey to elective surgery throughout the pathway.
- It has been shown that patients whose diabetes is well controlled before their operation are less likely to have complications and more likely to be discharged home earlier.
- The aim of this perioperative diabetes passport is to help patients and the healthcare professionals looking after patients ensure that they are in the best possible condition for surgery and to make sure they receive the most appropriate care during inpatient stay.
Access an amendable version of the Diabetes Passport for use in your trust
Adapted / Reproduced, with permission, from © Ipswich Hospital, East Suffolk and North Essex NHS Foundation Trust
The following resources are highly valuable for patients with diabetes undergoing day case surgery and staff treating patients on the day case diabetes pathway
Read CPOC's response here.
Here are recent technical guidelines from other collaborative groups. One on the use of technology and one for managing continuous subcutaneous insulin infusion (CSII, or ‘insulin pump’) therapy in hospitalised patients
A consensus statement from the Association of Anaesthetists, Association of British Clinical Diabetologists, British Obesity and Metabolic Surgery Society,
Centre for Perioperative Care, Joint British Diabetes Societies for Inpatient Care,
Royal College of Anaesthetists, Society for Obesity and Bariatric Anaesthesia and UK
Clinical Pharmacy Association

Dr Nicholas Levy is a consultant anaesthetist at West Suffolk Hospital and has had a keen interest in improving the perioperative management of surgical patients with diabetes for many years. He has contributed to all the previous major UK guidelines for the management of these patients and led the group that proposed that NCEPOD should conduct the aforementioned confidential enquiry. Like many anaesthetists he is also concerned that current guidance precludes the use of the continuous subcutaneous insulin infusion during surgery, and he is keen to see that the guidance navigates this contentious area for the benefit of patients.

Prof Gerry Rayman is a consultant physician at the Diabetes and Endocrine Centre and the Diabetes Research Unit at Ipswich Hospital, as well as an honorary professor at University of East Anglia, visiting professor at the University of Suffolk, associate lecturer at Cambridge University, Diabetes UK’s clinical lead for inpatient care and the Getting It Right First Time (GIRFT) joint clinical lead for diabetes. He also devised the national diabetes inpatient audit (NaDIA) programme. This annual quality improvement project has repeatedly demonstrated that harm to inpatients with diabetes predominantly arises from hospital acquired hypoglycaemia, hospital acquired DKA, and medication errors. One of the main aims of the guideline authors is to reduce the rate of these preventable harms.
We want to hear your feedback on the Diabetes Guideline
Please contact us to let us know your thoughts and questions




