Guidelines
Guidelines
In this section you'll find guidance developed by CPOC or guidance CPOC has produced in collaboration with other organisations.
CPOC produces guidance as an aid to support health care professionals in perioperative care. We use robust processes to develop our guidance taking into consideration expert opinion and the latest research.
CPOC develops its own guidance under the five strategic themes laid out in the CPOC Strategy 2023-2026. In this section you can view all the guidance CPOC has published or currently working on. CPOC aims to provide a bank of resources on all things perioperative care.
We regularly review our guidance on this website.
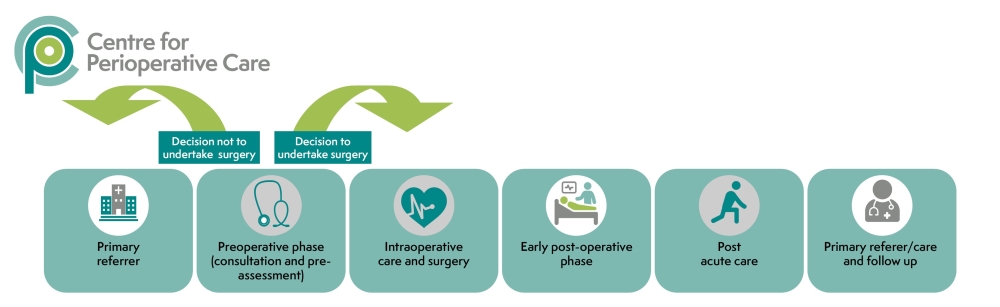
Our CPOC guidelines encompass the whole perioperative pathway and include recommendations for each distinct area across the perioperative journey.
CPOC Guidelines
Publications and Projects CPOC has Endorsed
Elective perioperative management of adults taking glucagon-like peptide-1 receptor agonists, glucose-dependent insulinotropic peptide agonists and sodium-glucose cotransporter-2 inhibitors
Association of Anaesthetists, Association of British Clinical Diabetologists, British Obesity and Metabolic Surgery Society, Centre for Perioperative Care, Joint British Diabetes Societies for Inpatient Care, Royal College of Anaesthetists and the Society for Obesity and Bariatric Anaesthesia
Publications & Projects CPOC Supports
Other Organisations Perioperative Guidelines
Perioperative Care for the Cystic Fibrosis Patient
Cardiff and Vale University Health Board
The guidance aims to provide a background knowledge of Cystic Fibrosis [CF] for the anaesthetist and give guidance and best practice for the perioperative anaesthetic management of the patient with CF presenting for surgery.
CF affects multiple organ systems. However, the impact of CF on the respiratory and gastrointestinal systems account for the majority of morbidity and mortality. Therefore CF patients are generally considered a high risk group for anaesthesia, particularly given their potential for postoperative respiratory complications.
Guidelines for the Provision of Anaesthetic Services (GPAS)
Royal College of Anaesthetists
The Guidelines for the Provision of Anaesthetic Services (GPAS) support anaesthetists with responsibilities for service delivery and healthcare managers to design and deliver high quality anaesthetic services. It is developed using a rigorous, evidence-based process, which was accredited by the National Institute for Health and Care Excellence (NICE) in 2016.
Each of the GPAS chapters should be seen as independent but interlinked documents. Guidelines on the general provision of anaesthetic services are detailed in the following chapters of GPAS:
- chapter 2: guidelines for the provision of anaesthesia services for perioperative care of elective and urgent care patients
These guidelines apply to all patients who require anaesthesia or sedation, and are under the care of an anaesthetist. For urgent or immediate emergency interventions, this guidance may need to be modified as described in chapter 5: guidelines for the provision of emergency anaesthesia.
Prehabilitation for people with cancer: Clinical and implementation guidelines
Developed in collaboration with the NIHR Southampton Biomedical Research Centre, the Centre for Perioperative Care, the Royal College of Anaesthetists, the NIHR Cancer Nutrition Collaborative and the World Cancer Research Fund.
These updated 2025 guidelines build on the original guidance published in 2019. These guidelines provide detailed, evidence-based recommendations for designing and delivering prehabilitation services for people living with cancer.
They aim to support widespread adoption of prehabilitation to improve patient preparation, recovery, experience of care and sense of control. They also include practical information to help healthcare provider organisations develop services tailored to communities they serve.
Read the Clinical and Implementation Guidelines
Prehabilitation for people with cancer
Principles and guidance for prehabilitation within the management and support of people with cancer
In partnership with Macmillan Cancer Support, The Royal College of Anaesthetists (RCoA) and the National Institute for Health Research (NIHR) Cancer & Nutrition Collaboration
Macmillan Cancer Support, the RCoA and the NIHR Cancer and Nutrition Collaboration in July 2019 launched a report calling for changes to the delivery of cancer care across the UK, with a greater focus on prehabilitation including nutrition, physical activity and psychological support.
Seventy per cent of the 1.8 million people in the UK living with cancer are also living with one or more other long-term health conditions. The guidance report, Prehabilitation for people with cancer, promotes evidence that when services are redesigned so that prehabilitation is integrated into the cancer pathway:
- patients feel empowered and quality of life is improved
- physical and psychological resilience to cancer treatments is maximised
- long-term health is improved.
Teams from Macmillan Cancer Support, RCoA and NIHR have worked together to develop these principles and guidance together with an action plan. This sets out how NHS organisations across the UK can replicate some of the pioneering work already taking place at a limited number of Trusts – all of which have demonstrated how prehabilitation has improved outcomes and reduced the risk of disease progression.
A review of the perioperative care of surgical patients
This report, released by NCEPOD in 2011, recommends that:
- There is a need to introduce a UK wide system that allows rapid and easy identification of patients who are at high risk of postoperative mortality and morbidity. (Departments of Health in England, Wales & Northern Ireland)
- All elective high risk patients should be seen and fully investigated in pre-assessment clinics. Arrangements should be in place to ensure more urgent surgical patients have the same robust work up. (Clinical Directors and Consultants)
- An assessment of mortality risk should be made explicit to the patient and recorded clearly on the consent form and in the medical record. (Consultants)
- The postoperative care of the high risk surgical patient needs to be improved. Each Trust must make provision for sufficient critical care beds or pathways of care to provide appropriate support in the postoperative period. (Medical Directors).
- To aid planning for provision of facilities for high risk patients, each Trust should analyse the volume of work considered to be high risk and quantify the critical care requirements of this cohort. This assessment and plan should be reported to the Trust Board on an annual basis. (Medical Directors) Principal Recommendations T
NICE guidelines on routine preoperative tests for elective surgery
The recommendations in this guideline represent the view of NICE, arrived at after careful consideration of the evidence available.
When exercising their judgement, professionals and practitioners are expected to take this guideline fully into account, alongside the individual needs, preferences and values of their patients or the people using their service.
It is not mandatory to apply the recommendations, and the guideline does not override the responsibility to make decisions appropriate to the circumstances of the individual, in consultation with them and their families and carers or guardian.
Being Active: An everyday guide for people living with an impairment or health condition
This guide, produced by the English Federation of Disability Sport, Disability Rights UK and Sport England, seeks to provide the information needed to support people living with a disability or health condition to become more active.
While the guide does not discuss the issues around every impairment or sport, it provides broadly applicable advice for people who wish to become more active and overcome the barriers that may be preventing them from doing so.
If you would like further information on the issues discussed in the guide, you can find out more by visiting the Activity Alliance website.
This GIRFT guidance is for non-medical pre-assessment leads, clinicians and managers, who want to embed best practice in their preoperative assessment processes. This guide should be used alongside the guide for earlier screening, risk assessment and health optimisation, the digital playbook for perioperative pathways, and local and national protocols.
UK Kidney Association
Acute Kidney Injury continues to pose significant challenges across healthcare, affecting nearly 600,000 people annually in the UK. This report provides a roadmap for addressing these challenges, transforming care delivery and fostering stronger connections across teams and disciplines.
Key highlights of the report from the National AKI Summit in 2023 include:
- Aligning AKI warning systems and data reporting to reduce regional disparities and drive targeted improvements.
- Enhancing collaboration across healthcare roles, including doctors, nurses, pharmacists, dietitians and laboratory professionals.
- Personalised, patient-centred approaches that integrate AKI care with broader chronic disease management.
- Clear pathways for safe transitions of care, preventing avoidable readmissions and stabilising long-term health.
If you have any ideas for future CPOC guidelines, please view our guideline proposal page.
CPOC Endorsement & Support
If you are interested in obtaining CPOC endorsement or support for your resource please read our policy and get in touch to discuss things further.