Using Strategy and Organisational Structure to improve Perioperative Care
Improving perioperative care requires a paradigm shift in how we provide care, moving from a specialty centred service to a pathway centred service. Significant challenges exist as the changes required straddle strategy, operations, finance, workflows, education and training, as well as all health and social care providers. Change is also required across multiple medical specialties.
Many of the drivers of this paradigm shift are anaesthetists or geriatricians with an interest in Preoperative Assessment (POA) or Perioperative Medicine. As such, we are well placed to influence our immediate environment: the anaesthetic service, POA and more recently Prehabilitation. However, to change pathways we need to influence multiple departments within our trusts, and multiple providers within our Integrated Care Systems. In addition to the groundswell of support from interested clinicians, we also need to influence strategy and organisational structure within our trusts and integrated care systems (ICS).
Strategy can be broadly described as a plan to achieve organisational goals. Every ICS will have a strategy, which will align with national strategic objectives in health and social care. Acute trusts will have a clinical strategy and multiple enabling strategies (digital, estates, education, people etc.).
Strategies aid communication between clinical and non-clinical functions (HR, finance, estates, transformation etc.). Most importantly, strategy determines allocation of resources and can lead to organisational structure change. Resources in this context means financial support for new roles, as well as dedicated support from transformation teams, digital etc.
Clinical services are invariably grouped into divisions (or care groups), and subsequently directorates, then departments, services etc. At the higher levels there is usually nursing, medical, operational, finance and HR input. The further down the hierarchy, the lower the representation and banding of each of these groups.
Clinical services may naturally fall within a particular directorate or division. However, some smaller services such as POA are added to a particular directorate’s portfolio based on head count, and therefore budget, or are added at the bottom of the hierarchy. These services therefore have relatively little input from senior medical, nursing or operational leaders. As many of the perioperative clinical leads are anaesthetists in POA, this makes it challenging to get enough support for such a big change programme.
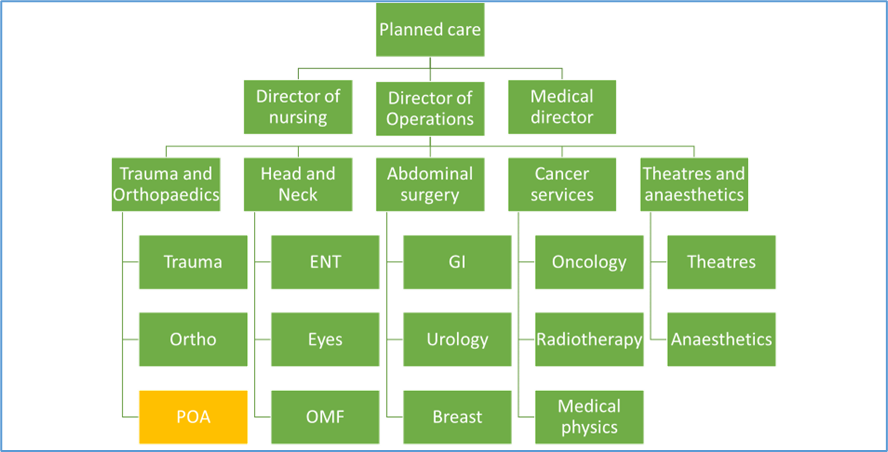
In 2018, POA at RBFT was under the directorate of Trauma and Orthopaedics. A simplified organogram is shown below. The service was predominantly managed by a band 7 nurse.
In 2018, perioperative medicine was first included in RBFT’s Clinical Services Strategy. The conversations around this led to a widespread agreement that the existing organisational structure was insufficient to support the strategy, and so, in 2022, the Clinical Director role for the existing Theatres and Anaesthetic directorate was expanded to include Perioperative Pathways (POA and Prehabilitation) and admitting areas. In 2023, the structure changed to create a new directorate, shown below.
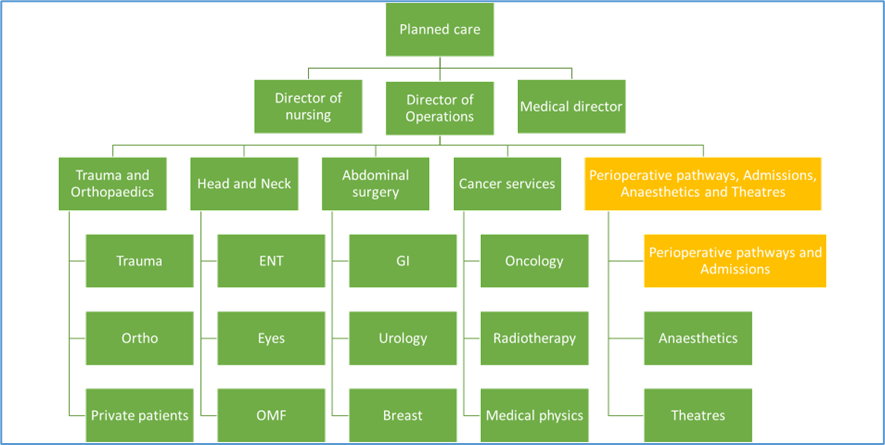
To support the new directorate, an additional matron (band 8b) was recruited to oversee Perioperative pathways (POA and Prehabilitation), and Admissions, and an additional 0.5WTE (band 8c) associate director of operations was recruited to support the entire pathway. The three subdivisions are managed by a directorate manager (band 8b) and two service managers (band 7). There are clinical leads for Anaesthetics, Theatres, POA and Prehabilitation. Within Theatres and Anaesthetics, there is a matron and three lead (band 8a) nurses.
The additional workforce, in combination with successful bids for NHSE and Macmillan grants, has enabled us to grow a prehabilitation service, support digital innovation to create efficiencies, and develop relationships with patient leaders, Primary Care Networks and stakeholders across the ICS.
Within our ICS, we have developed a network of engaged and invested individuals, from clinicians in acute trusts to members of the Integrated Care Board (ICB). Together with our strategy team, we have agreed a strategy for Perioperative Care across the ICS. This is evolving as the ICS matures but is a helpful starting point for aligning our goals.
Thanks to the efforts of national leaders in perioperative medicine, we have strategies and national NHS standards to support us from CPOC, GIRFT etc. However, we also need to drive a ‘bottom up’ change programme. Acquiring the personal skill set as a POA or Perioperative Medicine lead to influence strategy and organisational structure can be organic, or through specific leadership courses or qualifications (such as the NHS leadership academy, BA or MBA), but change of this magnitude requires a team of individuals; influencing strategy and organisational structure change is a way of building that team.
Dr Jennie Rechner. MBBS FRCA MSc BA
I have been a consultant anaesthetist at the Royal Berkshire NHS Foundation Hospital (RBFT) since 2008 with a longstanding interest in Perioperative Care. In 2023 I completed a BA in Applied Management with Henley Business School, using these skills to influence the trust’s strategy and organisational structure. I was appointed as Clinical Director in Perioperative Pathways & Admissions, Anaesthetics and Theatres in 2022.

