Development of a new ‘Post Operative Care Unit (POCU)’
In response to the pressures that COVID-19 put on our critical care services the idea for a new Enhanced Care Unit was devised at Kingston Hospital. The aim was to improve the quality of post-operative care, reduce surgical cancellations due to lack of ICU beds and provide a clear pathway for high-risk elective surgical patients. This led to the development of the Kingston Hospital Post Operative Care Unit (POCU).
This is a four bedded unit based on an elective surgical ward staffed by ward nurses with additional training (2:1 patient to nurse ratio) and supported by the Critical Care Outreach Team (CCOT). The unit is able to support invasive monitoring, epidural infusions and CPAP / Optiflow for patients at risk of undiagnosed OSA.
In order to develop this new unit, it was essential to get good buy in from all key stakeholders, including anaesthetic, ICU, nursing and surgical teams. All agreed the key objective was to improve post-operative care to high-risk surgical patients. A comprehensive SOP was developed based on national guidance and in response to local factors. This included a clear clinical review and escalation policy for all POCU patients. The key aim is to enable any early complications to be identified quickly and the appropriate care initiated efficiently.
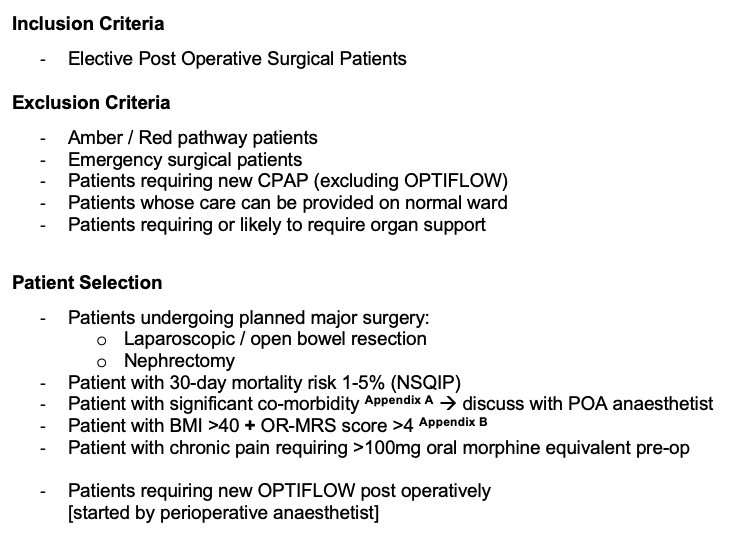
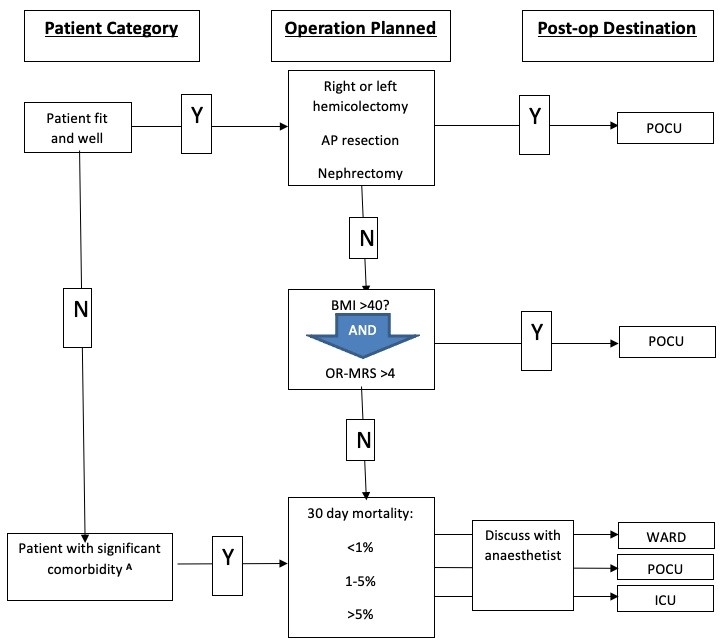
To ensure resources are allocated to the appropriate patients, a comprehensive booking criteria was established to ensure at risk patients are identified and beds requested in advance of surgery. This includes all patients undergoing major surgery, patients with a predicted mortality of 1-5% and those requiring urgent surgery at risk of undiagnosed OSA. POCU beds are booked by the Pre Operative Assessment (POA) team before the day of surgery. Extensive education sessions were done with the POA team to ensure appropriate patients are identified, including those patients who requite post-operative ICU rather than enhanced care.
Suitable patients are booked digitally in advance so all members of the perioperative team are aware. Patients can easily be moved to a new date if the operation has been changed or delayed. The anaesthetic lead for POCU has oversight over the booking process, so can assess suitability if needed and review patients if more beds are requested than are available.
A leadership team was also established to manage and organise the unit including nursing, anaesthetic and surgical members. This has meant urgent issues can be dealt with quickly and there is a clear decision making process. This has allowed practices to evolve and change quickly in response to local needs.
Since the unit was started in 2021, several new developments have been trialled and established. This includes the development of the digital booking system in January 2023. Prior to this beds were requested via email and added to a paper calendar. This meant it was difficult to confirm if a bed had been requested or share daily booking requests, leading to several late cancellation of bed requests.
A new Optiflow machine for specific use on POCU was bought by the Hospital Charity. This has meant further airway support can be offered to patients. Patients requiring Optiflow are managed by the POCU nurses with support from the CCOT team. In conjunction with this, a new SOP for post-operative Optiflow was developed allowing more patients to benefit from this intervention.
A new digital handover form has also been created. Post-operative patients transfer to POCU via the theatre recovery area, meaning there is no direct hand over from anaesthetist to ward team. The new handover form ensures a comprehensive handover of intraoperative events, medications and specific post-operative plans are provided for each patient.
There have also been challenges that have had to be overcome. The unit is located on an elective surgical ward, away from the main theatre area and ICU. This has meant a robust review and escalation policy had to be developed as anaesthetic and ICU teams cannot quickly see or review patients. All patients are reviewed daily by their surgical team and overnight by the on-call surgical team. The CCOT team provide valuable support and review every patient at a minimum every 12 hours and escalate to the ICU team as needed.
During 2023, 402 patients had a POCU bed booked, of which 68% end up requiring the post-operative bed. Most of those that didn’t require a bed were discharged as a day case. 11% of POCU patients required escalation and a review by the ICU team. However, all of these patients were managed on POCU and none required admission to ICU.
Dr Henry Lewith
Anaesthetic Consultant and Lead for Perioperative Medicine Kingston Hospital
Joint Medical Lead SW London Perioperative Transformation Programme
Dr Lewith undertook his anaesthetic training in London and Oxford, with subspeciality training in Cancer & Bariatric Surgery. He completed a Perioperative Medicine fellowship at The Royal Marsden Hospital and has an interest in the optimisation of patients undergoing surgery.

